Drug resistance is threatening the control of tuberculosis (TB) in South Africa and other parts of the world, but no one knew exactly where XDR-TB came from.
This was until recently when scientists from the KwaZulu-Natal Research Institute for Tuberculosis and HIV (K-RITH), the Broad Institute of MIT, and Harvard in the US traced the roots of extensively drug-resistant TB, aka XDR-TB in KZN to the late 1950s.
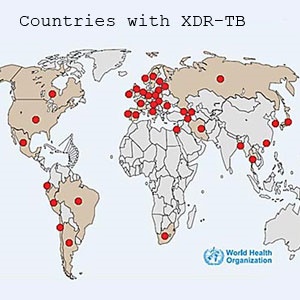
These new findings, which were published in the journal PLOS Medicine on 29 September 2015, have important implications for the way we understand how XDR strains are spread, as well as for the management and treatment of TB across the world.
In XDR-TB, the bacterium that causes TB has become resistant to nearly all currently available anti-TB drugs.
K-RITH scientist, Dr Alex Pym, a lead author on the research paper, explains that XDR_TB is currently treated with a combination of poorly active third-line drugs for two years or more, but is associated with a very high mortality (>50% death rate).
Bedaquiline (a new drug) and linezolid (a drug used to treat other drug resistant bacteria) offer some hope, but these are not yet available to all patients who might need them in South Africa.
The main reason for this is because clinical trials aren't concluded, and the drug can be prohibitively expensive.
This leaves healthcare workers with limited treatment options for people infected with these strains.
The largest outbreak of XDR TB in history was first detected in KZN in 2005 at the Church of Scotland Hospital in Tugela Ferry, where it killed 52 out of 53 people infected. XDR TB is now found throughout the province.
Up until now it was not known where XDR TB came from.
How researchers traced XDR-TB
The researchers used genome sequencing to trace the origin of XDR-TB in KZN. Genome sequencing is simply when they work out the entire genetic code of an individual strain of bacteria and then date the analysis.
Looking at the analysis, they found that the mutation in the TB bacteria that cause drug resistance emerged in 1957, soon after the first antibiotics to treat the disease became available.
Since then, every time a new drug was introduced the TB bacteria successfully developed resistance to it.
By the 1980s, the microbe had evolved to multi drug-resistant status (MDR), and by the mid-1990s it had mutated to XDR.
This means that the massive problem of drug resistance in South Africa is not due to recent challenges in TB control. It also shows that it developed well before the explosive HIV epidemic in the 1990s, which was previously thought to be the cause of XDR-TB in KZN.
During the process of tracing the Tugela Ferry XDR strain, researchers also found many other strains of drug resistant TB that were evolving independently of each other.
Vitally, scientists discovered that the first drug all the strains develop resistance to was the antibiotic isoniazid. This was the key step that started the evolution towards XDR.
When doing rapid tests for MDR and XDR-TB, most hospitals and clinics in South Africa currently only test for resistance to the drug rifampicin.
Note: Rifampicin was discovered in 1957, and received approval for therapeutic use in 1968 as part of a combination of medicines to treat TB. It remains one of the strongest medications available for TB treatment. Patients who are resistant to both rifampicin and isoniazid have MDR TB.
How to stop the evolution of resistance
What is critically important right now is to stop the further evolution to new resistance. One way researchers believe that can be done is by making screening for isoniazid resistance mandatory.
Dr Alex Pym said: “If we want to turn off the tap to generating new drug resistant strains of TB, we have to screen for isoniazid resistance as well.”
He explains that, at the moment, all patients in South Africa are tested for rifampicin resistance (GenXpert). If they are not resistant to this, then no further testing is done and they get started on first-line therapy.
"But our study shows that in every case isonaizid resistance was the first step in developing XDR-TB. So, unless we also detect isoniazid resistance early and treat it properly, we are sowing the seeds for further drug resistance."
He added: “There is some real hope for treating XDR as this year the National TB Control Programme was able to get access to the first new TB drug developed in 40 years – called bedaquiline – and there are others in the pipeline.
"But unless we use these new drugs extremely carefully, the XDR-TB bacteria will continue its relentless evolution and the new drugs will become useless.”
Dr Pym explains that this is because TB is like HIV. "If you treat the disease with only one drug, the bacteria can rapidly develop resistance to it. If we use a combination of drugs, it is very unlikely that the bacteria can develop resistance simultaneously to all drugs," he says.
Also, if patients don't take their drugs regularly and correctly the bacteria is likely to develop resistance.
Why has it taken 40 years to develop a new anti-TB drug?
"Pharmaceutical companies don't see a large enough market to invest in TB compared to chronic diseases that that affect people in affluent countries. As a result, there was little investment in TB drug development," says Dr Pym.
"TB is largely a disease of less developed counties. Also, it was assumed that TB would go away with increasing living standards as it has done in Europe and USA. Finally, the rise of drug resistant TB was ignored."
How should drugs be administered?
"When we start using a new drug, it's essential that it's only given with at least one or two other drugs that the bacteria are not resistant too," says Dr Pym. "Patients need to be assessed very carefully in combination with drug resistance testing before being given a new drug to ensure they get given an effective combination.
"If this is not done, resistance to the new drug will develop rapidly, as it has done over the last 40 years, and we will be back to where we started."
By tracing XDR-TB can we stop the evolution of TB?
"It was assumed that the problem of XDR-TB in South Africa was due to recent failings in the TB control programme in combination with HIV. But this study shows that resistance had actually started evolving right from the introduction of the first antibiotics to treat TB, and once resistance emerges it doesn't go away and continues to be transmitted.
"So, if we are going to halt or at least slow down this process we need to introduce new combinations of drugs rather than just one drug at a time.
"This will require very careful "antibiotic stewardship" – i.e. careful control of how new drugs are employed, as well as an acceleration of new drug development."
What's been wrong with TB treatment up to now?
"The problem has been that there hasn't been enough new drug development, rather than the type of development. So now we are faced with only having one new drug and how to employ it.
"Tracing the origin of drug resistant TB and how easily resistance can become fixed in a population highlights the urgency of the new drug development.
"In a sense, the TB bacteria can evolve faster than we can develop new drugs."
Why look at the resistance to isoniazid to unravel XDR-TB?
"Actually we didn’t. We took a whole range of drug resistant bacteria and did our genetic analysis.
"This allows use to trace the last common ancestor of the drug resistant strains. It's a bit like drawing a family tree based on genetic differences.
"What we found was that if you trace the origin back to the last common ancestor it was always isoniazid resistance that was the first drug to which all the strains of TB became resistant."




 Publications
Publications
 Partners
Partners










