Alternative Names:
Skeletal X-ray, X-ray joint
What is a Joint X-ray?
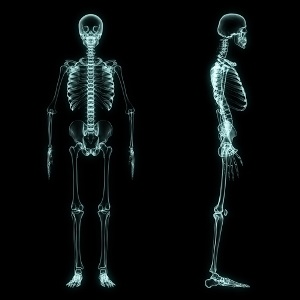
It is a plain X-ray of one or more joints of the body, e.g. hip, knee, ankle, elbow, shoulder and wrist, which are the most common joint X-rays.This means that X-rays (a form of electromagnetic energy like light that can travel through the body) are used to penetrate your 3D anatomy and capture the image on a flat 2D X-ray film, placed on the opposite side of your body.
Depending on what your doctor suspects, he may order one or more views of the joint, i.e. antero-posterior or frontal view, lateral or side view, and any oblique projection or different positions of the joint, for example bent or extended knee, shoulder turned in then outward, or hips that are bent upwards and turned outwards.
The same joint on the other side of the body may be X-rayed as well for comparison (especially in children), or if the abnormality is suspected on both sides.
A skeletal survey is sometimes performed on combinations of joints to look for the presence of joint diseases that affect specific joint combinations. Changes may be found in one or more of the imaged joints, confirming the diagnosis of a disease affecting multiple joints.
How is the procedure commonly used?
It is most commonly used after injury to look for fractures, dislocations or bleeding in the joint.Joint X-rays are performed to look for diseases of joints, which present as constant pain in a single or multiple joints, visible deformity or joint changes, redness and swelling, as well as a decrease in joint function, e.g. inability to fully extend or bend joint or inability to stand due to joint instability or pain.
Once a serious chronic joint disease has been identified, e.g. rheumatoid arthritis, a routine X-ray of all the joints affected by the disease and likely to be affected by it in the future may be done in order to assess the extent of the current health of the joints. It may be repeated at regular intervals to monitor the progression of the disease. Joint destruction, for example, which is progressive, may necessitate more aggressive treatment to stop the disease process.
X-rays are frequently used after orthopaedic surgery to assess the changes in the joint and to look for complications after the surgery. Examples are infection, malalignment of bones, or loosening, migration or failure of orthopaedic implants, like joint replacement prostheses, plates, rods and screws.
Joint X-rays are used in newborns and infants if skeletal birth defects or bone abnormalities like achondroplasia or osteogenesis imperfecta are suspected.
How should I prepare?
Make sure you wear clothing that can be removed or pulled away from the joint being X-rayed. If you normally wear jewellery like rings and bracelets near the joint, rather leave them at home, as they would have to be removed for the procedure and may get lost.How is the procedure performed?
After registering at the X-ray Department and spending some time in the waiting room, you will be led through to the X-ray room, which has a bed and an X-ray machine. The joint is then exposed from under your clothing, and any jewellery or other metal objects like braces, splints removed (if possible) if they are in the way. The joint is positioned between the X-ray cassette, which is a flat plastic cassette that holds and protects the X-ray film, and the X-ray tube, the machine that produces the actual rays that will travel through your body onto the X-ray plate to form the image.Newer X-ray departments may use digital X-ray machines. This means that the joint is positioned on a flat panel sensor. A beam of light is used to help position the limb, X-ray cassette, and X-ray tube overhead.
The image is then taken. It is entirely painless and feels the same as having your photograph taken! Afterwards the joint may be repositioned for X-rays from different positions or angles.
Risks
The greatest risk is to the pregnant patient. It is dangerous for the developing foetus to be exposed to X-rays, as this may cause abortion or serious birth defects. So, if you are pregnant or suspect that you may be, you should inform the X-ray department so that the procedure can be postponed to after the birth of the baby, or if it becomes certain that you are not pregnant.The X-ray poses no immediate danger to your health. There is no clear evidence that X-rays in average doses increase one’s risk for cancer, therefore having an X-ray is considered entirely safe.
What are the limitations of the procedure?
X-rays do not show different soft tissues like ligaments, tendons, cartilage, synovial or bursal membranes well, therefore pain from or disease of these parts may not show up on an X-ray. Cartilage thickness (joint space) and osteoarthritis progression may be estimated from an X-ray, but once again the actual cartilage cannot be seen.Due to overlapping or blurring of shadows on the X-ray picture, small bone fractures may sometimes be missed. Sometimes a bone defect, lesion or fracture may incorrectly be displayed where there is none, once again due to overlapping shadows or “artefacts”, which are false non-anatomical structures that can be appear on the final X-ray image. This may be caused by incorrect film handling or problems in processing, similar to those found in photography, e.g. spots, lines and fingerprints!




 Publications
Publications
 Partners
Partners











