Definition
A pacemaker is a small, battery-operated device implanted into the body to regulate the heartbeat.
Normal heartbeat regulation – and problems encountered
The regular synchronised contraction of all four chambers of the heart is regulated by electrical impulses generated within a group of specialised cells in the heart, called the sino-atrial node (SA Node). The impulse generated at the SA Node causes the atria to contract. It then passes to the “sub-station”, the atrio-ventricular node, which carries it into the conduction system of the ventricles. These impulses are carried along special conducting tissues – similar to an electrical wiring system – called the Bundle of His and the Purkinje fibres. These fibres are arranged for optimum performance of the heart, for example the atria (or receiving chambers) contract a split second before the ventricles (the pumping chambers), allowing them to fill the ventricles as much as possible between beats.
The SA Node is sensitive to changes in the body – heat (such as a fever), exercise or stimulant drugs will cause it to “fire” more often, and speed up the pulse rate. In the same way, other factors can slow the pulse. This responsiveness is vital, allowing the body to adapt to the varying demands made, and ensuring optimum cardiac function.
The SA node and all the components of the conduction system may also be affected by degenerative changes and diseases, which can affect only certain parts, or all of the system. The result is a disruption in the normal rhythm of the heart, called a dysrhythmia. This problem may be intermittent at first, and may later become permanent.
There are different types of rhythm disturbance, each with its own problems. For example, atrial fibrillation (AF) can leave a person feeling weak and unwell, and predisposes towards clots forming in the heart chamber itself. Parts of these clots can break off and be carried to the lungs or brain, causing a stroke, or a (possibly fatal) lung embolus. Ventricular fibrillation causes the ventricles to quiver ineffectively instead of pumping efficiently, and is rapidly fatal if unrecognised and not immediately corrected by defibrillation.
Why are pacemakers inserted?
From the above description of the normal conducting system, it is clear that problems may arise at any point. Regardless of where the problem arises, or what its cause is, the end result is an abnormal pulse – too slow or dangerously irregular. Some patients do not respond well to medical treatment, and others may have a condition which is simply not treatable by any medical means. Yet another group of patients may have a combination of an irregular pulse which tends to degenerate into a potentially fatal fibrillation. For all of these patients, a pacemaker can be used.
A pacemaker does not cure the underlying condition, but allows the patient to live with it.
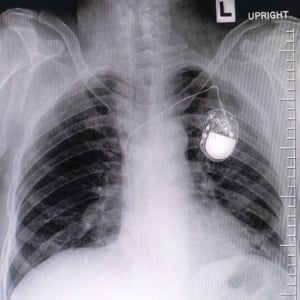
What does a pacemaker consist of?
Simply put, a pacemaker consists of three basic elements:
- A generator, which combines the power source – a high-tech battery – and the computerised information controlling the work of the pacemaker. These generators are compact and light, weighing about 30-40 grams, and have a life span of 7-10 years, after which they need replacing.
- Leads carrying electrical impulses to and from the heart chambers.
- Electrodes/s and sensors at the tip of the lead/s which connect with the heart. The sensors are used to detect the intrinsic electrical activity (rhythm) of the heart, while the electrodes can deliver to the heart muscle the electrical impulse generated by the pacemaker’s battery.
There are different types of pacemakers, each for a specific category of problem. Examples of these are:
- Single chamber pacemakers – a single electrode stimulates a chamber to contract. Placed in a ventricle, this may be used to prevent very slow heart rate. Used in the atrium, it may be effective if the sino-atrial node malfunctions, but the rest of the conduction system is intact and can be used to conduct impulses from the pacemaker.
- Dual chamber – here, electrodes use low-energy impulses to stimulate both the atria and ventricles to contract, mimicking as far as possible the natural cycle of events.
- Biventricular – this paces both ventricles, and is technologically more complex and difficult to insert. This is starting to be used more often in the management of heart failure in selected patients.
- Internal cardioverter/defibrillators (ICD)– these can function as pacemakers, but can also detect the onset of dangerous rhythm disturbances. In these instances, they can function as defibrillators. This is used for certain categories of patient only, mainly those whose condition places them at risk of fatal fibrillation.
Pacemakers can be programmed to sense certain abnormal rhythms, and to respond in a variety of ways. For example, they can be set to maintain a fixed pulse rate. Or they can be programmed to only pace if the pulse rate drops below a certain speed. The ICDs can be programmed to detect the abnormal rhythm, start to pace at low energy, then, if the abnormal rhythm persists or degenerates into fibrillation, to deliver a corrective, high-energy shock.
Pacemaker insertion – procedure, complications and risks
Insertion of a pacemaker is a surgical procedure, performed under sterile conditions in a special theatre. An area of skin just under the collarbone is deadened using local anaesthetic. A small incision is made, and a “pocket” is hollowed out of the tissues, to receive the generator/battery. A nearby large vein is then used to thread the electrodes into the heart: special X-ray monitors are used to ensure the correct positioning of the tips of these electrodes. When correctly positioned, the electrodes are connected to the generator. The skin is then closed.
As with any operation, there are possible complications. Because this procedure does not need general anaesthesia, the possible complications of breathing problems do not apply, but the basic risk of bleeding remains.
There are specific complications associated with pacemaker insertion, though, and they include
- uncontrolled bleeding at the vein puncture site
- puncture of the heart leading to blood collecting in the pericardial sac – this may need urgent surgical drainage. This is an uncommon problem.
- abnormal heart rhythms may be caused by the electrode tip irritating the heart muscle during insertion/placement.
- pneumothorax (dropped lung) may occur, especially in very thin patients. Not a common problem fortunately.
- infection is the most feared complication, and may affect either the pocket or the leads, or both. The source of the infection may be the procedure and apparatus itself. Alternatively, infections elsewhere in the body, such as bladder infection, can lead to bacteria settling on the equipment. The infection may then track back into the heart, where the deadly condition of endocarditis may develop.
There are also certain circumstances and underlying medical conditions of the patient which increase the risk of complications occurring. These include
- diabetes mellitus
- underlying malignancy
- advanced patient age
- recent/current use of anti-coagulants or glucocoticoids (warfarin, cortisone)
- recent surgery involving the device greatly increases the risk of infection
- operator inexperience increases the risk of all complications
Precautions
Because pacemakers are electromagnetic devices equipped with sensors, and are designed to respond to information detected by these sensors, there is a risk of malfunction if other electromagnetic apparatus in the environment interferes. Most modern pacemakers are adequately shielded, so that patients can lead normal lives with only a few restrictions.
Household/kitchen equipment is generally not a threat. Most microwaves and TV sets do not interfere with the working of the pacemaker. The new induction cooker tops may cause problems if a pot is not symmetrically placed on the heating area, or if the patient stands too close to the stove.
Cellphones in normal use cause no problems. However, cellphones should not be carried in a breast pocket near the generator – the greatest risk is during the ringing phase, when signal strength emitted is at its maximum and may interfere with the generator.
Security systems such as those used in banks, shopping centres and airports are safe, provided that the patient walks briskly through them, and does not linger or get close to the source of the signal.
MRI scans are contra-indicated for patients with pacemakers. Fortunately, there are many other excellent types of scans and imaging procedures available for diagnostic purposes.
Shock lithotripsy – the use of external high energy sound waves to crumble kidney stones - is not recommended for patients with ICDs. Some of these have sensitive Peizo-electric crystals which can also be shattered, rendering the device useless.
Other considerations
Depending on the original cardiac problem, blood-thinning medication may need to be used. This may increase the likelihood of bleeding near the pocket, with even minor trauma.
Regular checkups are needed to verify that the pacemaker is working correctly, and that sensors and leads are intact.
The generator/battery unit will need replacing after several years. This means another minor operation, which carries further risks of complications. Leads are not replaced unless they are proven to be faulty or infected.
Because the whole pacemaker unit constitutes foreign material implanted directly into the heart, patients must inform any attending doctor or dentist of its presence. Ideally, patients should carry a MedicAlert tag of some kind.
Any patient with a pacemaker who experiences vague symptoms of fever, fatigue and general malaise must be regarded as having primary or secondary infection until disproved. Signs of local infection of the pocket may be found. If not, a blood culture test will be needed to identify the bacteria in the blood, and determine their sensitivity to antibiotics. If bacteria are present in the blood, they may infect a heart valve, causing infective endocarditis, a serious, potentially fatal condition if untreated.




 Publications
Publications
 Partners
Partners













