Many people with incontinence are hesitant to see a doctor as they feel embarrassed, believe their incontinence cannot be treated, or are convinced that the problem will eventually go away by itself.
The good news is that, in most cases, incontinence can be successfully treated or managed. The treatment depends on the cause, the type of incontinence, and the severity of the problem.
Stress incontinence
Non-medical treatment
This includes:
- Weight loss
- Smoking cessation
- Pelvic floor exercises
- Using vaginal weights to retrain the pelvic floor muscles
- Biofeedback (i.e. a technique that teaches you to control your body’s functions)
- Electrical stimulation
Non-medical treatment can be very effective in motivated individuals who experience only minor degrees of stress incontinence. The short-term results are often good, but this isn’t always maintained in the long term.
Research shows that improvement rates are in the range of 50-80% for those who use pelvic floor exercises as a way of treating stress incontinence.
Medical treatment
Medical treatment doesn’t have much of a role in the treatment of stress incontinence. But, depending on the cause, the following may be prescribed:
- Oestrogens (e.g. Premarin cream)
- Alpha-agonists (e.g. duloxetine)
- A combination of the above
Postmenopausal atrophy (the wasting away of tissue) can affect the closure of the urethra (the bladder tube). Locally applied oestrogen can help to restore the bulk of the urethral tissue, leading to more effective closure of the urethra. Note that oral oestrogen formulations shouldn’t be used only for this purpose.
A class of drugs called the alpha-agonists can increase the tone in the bladder neck, thereby increasing outflow resistance in people with stress incontinence. But this medication isn’t routinely used, and surgical options provide more reliable outcomes for stress incontinence.
Surgical treatment
This may involve:
- Periurethral injections of bulking agents
- Suspension operations
- Sling operations
- Artificial urinary sphincters
With periurethral injections, bulking agents are injected into the urethra to improve urethral closure. Bulkamid, which contains polyacrylamide hydrogel (PAHG), is currently in use as a bulking agent.
Injection therapy is suitable for women with intrinsic sphincter deficiency (weakness of the urethral sphincter) rather than urethral hypermobility (where there’s too much movement in the urethra). It’s also suitable for men who have had surgery or radiation for prostate cancer and who now suffer from incontinence as a result (this is called post-prostatectomy incontinence).
The major advantage of injection therapy is that it’s a minor procedure. Short-term results are good but, unfortunately, aren’t always maintained in the long term.
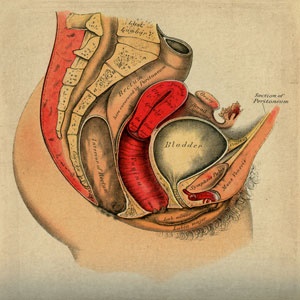
Various suspension operations are also used to restore the normal anatomy in people with hypermobility of the urethra, improving the support of the urethra and the bladder neck.
An open or laparoscopic colposuspension operation (or Burch colposuspension) provides the best long-term results. But since the vaginal sling procedure is a fairly simple yet equally effective operation, colposuspension is now reserved only for those people who don’t want to use synthetic tapes. Colposuspension should only be done by an experienced surgeon, preferably a doctor who performs this procedure often.
Urethral slings can be used in people with intrinsic sphincter deficiency as well as those with hypermobility. It involves the insertion of a strip of tissue or an artificial substance to support the urethra and bladder neck like a hammock. It increases outflow resistance and improves urethral closure by supporting the mid-urethra.
The vast majority of people respond very positively to this procedure, but the operation may make it difficult to pass urine for a while afterwards. Other complications include infection and erosion of the synthetic sling material, which then has to be removed.
Artificial urinary sphincters are made of silicone and can be used in people with total incontinence that resulted from irreparable damage to the sphincter. The artificial sphincter consists of a small cuff that’s placed around the urethra and a reservoir (balloon) that’s placed in the lower belly, next to the bladder. Both of these are connected with a small tube to a valve placed in the scrotum, which you then use to inflate or deflate the cuff.
Artificial urinary sphincters are very effective but they’re quite expensive, and there’s a risk of infection and erosion of the synthetic material. For this reason, it’s reserved for individuals in whom previous surgery has failed. If you have an artificial urinary sphincter, you’ll also have to go for regular check-ups for the rest of your life.
Urge incontinence
Non-medical treatment
This may involve:
- Bladder training
- Biofeedback
- Pelvic floor exercises
Bladder training involves urinating by the clock, and progressively increasing the time between voids. This can improve symptoms in people with urge incontinence and otherwise normal bladders. It can also be combined with biofeedback (which helps you to retrain and strengthen your pelvic floor muscles) as well as pelvic floor exercises.
Medical treatment
This may involve the use of:
- Oxybutynin
- Tolterodine
- Imipramine
Drug therapy forms the mainstay of treatment for people with urge incontinence that occurs as a result of bladder instability. These anticholinergic agents (substances that block the neurotransmitter acetylcholine in the nervous system) relax the bladder muscle and increase bladder capacity. Possible side effects include a dry mouth, constipation and blurred vision.
Surgical treatment
Injection of botulinum A toxin (botox) into the bladder muscle (detrusor) can be used if urge incontinence is the result of a neurological disease that causes overactive bladder contractions.
Tiny bladders (a result of radiation or tuberculosis) can also be enlarged surgically. During this procedure, a segment of the intestine is patched onto the opened bladder, thereby increasing the bladder’s capacity. Individuals with unmanageable bladder instability, who have failed other medical treatments, can also be treated in this way.
- Overflow incontinence
Overflow incontinence due to bladder outflow obstruction is treated by surgically removing the obstruction. The most common example is that of a man with an enlarged prostate who is treated by resection of the prostate gland (a procedure in which excess tissue is trimmed away).
If the incontinence is due to failure of the bladder to contract, then clean intermittent self-catheterisation (CISC), which involves putting a catheter in and taking it out several times a day, is the most appropriate treatment. Permanent indwelling catheters should be avoided, if possible.
- Total incontinence
Total incontinence due to a vesicovaginal fistula (an abnormal passage between the bladder and the vagina) or a ureterovaginal fistula (a passage between the distal ureter and the vagina) is treated by surgically repairing the defect.
Treating faecal incontinence
Once your doctor has established the underlying cause of faecal incontinence (FI), he or she will decide on the most suitable treatment. This could involve a combination of medication, exercise and other treatment methods.
Treatment options include:
Dietary changes: If your FI is caused by diarrhoea or constipation, making changes to your diet may help to normalise and regulate your bowel movements. Your doctor may ask you to keep a food diary to monitor the impact of dietary changes. For example, he or she may suggest that you increase your intake of high-fibre foods and fluids, or that you eliminate foods that may make the problem worse.
Medication: Your doctor may recommend specific medication or bulking agents (e.g. fibre supplements) to change your stool consistency. This will depend on whether you suffer from diarrhoea or constipation. Another option is Solesta, an FDA-approved gel that’s injected into the anus and which effectively reduces or completely treats FI in some people. This gel narrows the anal opening by bulking up the rectal tissue.
Bowel retraining: This routine encourages normal bowel movements and helps individuals with FI to achieve greater control by becoming more aware of the need to use the toilet. It may involve various actions, such as making a conscious effort to have a bowel movement at a specific time of day or using suppositories to stimulate bowel movements.
Biofeedback: This technique improves the strength and coordination of the anal muscles that help you to control your bowel movements. It also heightens the sensation related to the rectum filling with stool. Biofeedback is usually taught by a specially trained physiotherapist who shows you how to do simple exercises to strengthen your pelvic floor muscles, how to sense when stool is ready to be released, and how to contract the muscles if it’s inappropriate to have a bowel movement at a specific time.
Kegel exercises: Also called pelvic floor exercises, these exercises focus on strengthening the muscles of the anus, buttocks and pelvis. When done correctly, they can be effective in improving or resolving your FI. They involve a routine of repeatedly contracting the muscles used when making a bowel movement. Kegel exercises should be done in a series of 30 contractions, three times a day. They usually strengthen the pelvic floor muscles within a few weeks.
Surgery: If you don’t respond to other treatments ,or have an underlying condition that’s causing FI, surgery may help you to regain control. There are various surgical options available.
When to call your doctor
Check in with your doctor if:
- Home treatment and lifestyle changes don’t provide sufficient relief.
- You notice blood in your urine or stools.Urinary incontinence (UI) is accompanied by pain, or you sense incomplete emptying of the bladder.
- UI is associated with a sense of heaviness or a bulge sensation in the vagina.
- Your incontinence gets worse.
- UI begins suddenly.
- Incontinence first occurs after a recent gynaecological operation or another operation that involved the organs in the pelvic area.
- Incontinence started or worsened soon after starting to use a specific medicine, e.g. after starting treatment for depression, heart failure or Parkinson’s disease.
- Incontinence is associated with body weakness. This can be a sign of a serious, underlying problem like stroke.
- You’re experiencing incontinence and you had pelvic radiation therapy in the
What is the course and prognosis of incontinence?
Urinary incontinence (UI) and faecal incontinence (FI) can be cured or improved in most people. In fact, with modern treatment methods, the cure rates are very high.
The ongoing improvement in medical technology, as well as the recent equipping and professionalising of doctors with a keen interest in pelvic-floor conditions (a super-specialised field dealing with incontinence), means that affected individuals should no longer accept to silently experience this problem. The key to recovery is to become an active participant in the prescribed solution.
Other than the social impact of untreated UI, prolonged contact with urine can, for example, result in contact dermatitis and skin breakdown. The exposed skin area may end up infected, resulting in severe medical complications. It’s therefore crucial to get proper treatment.
Talk to your doctor about the treatment option that’s right for you. Your treatment plan will be tailored to the type of incontinence you have, as well as your specific causes and symptoms.
Read more:
Risk factors for incontinence
Reviewed by Dr Dakalo Muavha, Specialist in Obstetrics & Gynaecology, MBChB DipObs FCOG Mmed, University of Cape Town and Groote Schuur Hospital. May 2018.




 Publications
Publications
 Partners
Partners














