AFTER her own battle against breast cancer Wilma van der Bijl, still as gorgeous as when she was crowned Miss South Africa in 1987, is now reaching out to other women who have cancer.
Wilma lived through some of her darkest moments when cancer was diagnosed in June 2005. Shortly thereafter she underwent a double mastectomy.
She’s outspoken about what she has been through and is keen that other women have regular breast examinations and do everything they can to stay healthy.
Although her cancer was picked up while still in the early stages she was shocked when she was diagnosed.
“I didn’t fit the profile at all,” she says. “I was 42 at the time and in good health – I don’t smoke, I’m not overweight and cancer doesn’t run in my family so I had no reason to suspect I might be at risk. But just before diagnosis I was tired all the time and no matter how much I slept it was never enough.
At the same time my right breast didn’t feel 100 per cent. I think subconsciously we’re aware of what’s going on in our bodies and breast cancer served as my wake-up call.”
But a mastectomy followed by a bout of chemotherapy is bound to knock any woman’s strength and it’s hardly surprising that after her treatment Wilma’s strength of character was tested to the limit.
“I suffered really bad depression and severe complications from the chemotherapy,” she recalls. “But my children were six and seven at the time and even though I felt absolutely sick and spent I knew I had to find the resolve to live for them and my husband.”
Even then it took all the strength she could muster when doctors found she had ductal carcinoma. “Losing a breast couldn’t compare with the alternative of death. I’m more than just a breast.
“I know it might sound peculiar and many people won’t relate to this but I’m glad for the warning. I take much better care of myself now and make sure I live every day to the full. Whenever I can I encourage other women to get checked on an annual basis. Th e inconvenience of a mammogram is nothing compared with the drama and anguish of a mastectomy.
“I’m so glad my cancer was diagnosed early. If it had been any later the consequences would have been much more serious. I’m also grateful I opted for reconstructive surgery immediately after the mastectomy and would urge other women to seriously consider this option.
Just like Wilma, Melléta Louw (53) was blindsided by a diagnosis of breast cancer.
This psychologist from Wellington was devastated when she heard she had cancer in April 2003, but says her journey was one of growth that left her with a new sense of hope and wonder.
One evening in January 2003 Melléta discovered a tiny lump in her breast while in the bath. It was so small she thought she was imagining things and went for a mammogram only three months later. The lump was malignant.
“The surgery to remove the lump and glands was pretty painful, as were the weeks that followed,” Melléta says. “But I was blessed in that I never felt ill or nauseous during my six weeks of chemotherapy.
“I read everything I could find on breast cancer. The knowledge helped me to face the treatment without fear. I shaved my head before my hair could start falling out. I wore bright bandanas and beautiful hats decorated with flowers and still felt attractive.” The seven weeks of radiation therapy that followed were nothing compared to the operation and chemo.
“That December was my best Christmas holiday ever. My treatment was over. I still felt drained but looked at the sea, the sand and the children playing with fresh eyes.
“I embark on the road ahead with gratitude and with a heightened awareness of the world around me. If I could tell other women diagnosed with breast cancer just two things it would be to take responsibility for their own health and to rest a lot during treatment.”
Sadly, unlike Wilma and Melléta, Tarryn Smith – who turns 34 in September – wasn’t diagnosed early and for her the delay has had dire consequences.
Tarryn was just 26 when she had to undergo a double mastectomy followed by months of chemotherapy. She is currently on Herceptin, a new drug used to treat a particularly virulent form of breast cancer. “When I was 26 I became aware of a lump in my breast but breast cancer was the last thing on my mind. According to my GP and the specialist surgeon who examined me I was too young to have breast cancer.”
The surgeon didn’t do a mammogram or a biopsy because as far as he was concerned she was off the breast cancer radar. Th is was despite Tarryn’s strong family history of breast cancer.
In the space of a year the tumour had grown from 1 cm to more than 4,5 cm and had spread to the glands in her armpit. Her doctor referred her to a plastic surgeon to have the lump removed. Within three days she had a radical mastectomy and her life changed forever.
The lesson for all women is that doctors can make mistakes. Trust your instincts. Get more opinions. If you feel uneasy don’t stop asking questions. Th e next six months were the worst time of Tarryn’s life. “I was battling the disease, undergoing really strong chemotherapy and trying to hold down a demanding job.
“I reported my GP and the first surgeon to the Health Professionals Council for medical negligence,” Tarryn says, “but the case went nowhere.” When she turned 30 the cancer reappeared, this time in her lungs. “I was devastated,” she recalls. “Strangely it was worse than the initial diagnosis because I assumed that once I’d been treated that would be the end of it and I would stay in remission. Nobody warned me there was a good chance the cancer would reappear. But a section of my lung was removed and I faced another round of chemotherapy. It was clear then that I was on a long and painful journey.”
People often find that when they undertake this journey with hope and courage there comes a hoped-for turning point in treatment that is exactly right for them.For Tarryn it has been the drug Herceptin, currently the drug of choice for treating Her2 metastatic breast cancer. Her2 is a gene that helps control how cells grow, divide and repair themselves.
“Herceptin is extremely expensive but enormously effective,” Tarryn says.
“Medical aids were reluctant to approve the drug and my dad was going to sell his house to fund my treatment but at the last minute the medical aid conceded.
“I’ll probably remain on it for a while longer. Th e medical aid will pay as long as I stay in remission. My cancer returned after three years so as I come up to the next three-year mark after my last surgery I’m really anxious. After fi ve years your chances of relapse diminish so this time I’m hoping I have a better prognosis.”
Unlike Wilma, Tarryn doesn’t regard cancer as a blessing in disguise or a wake-up call.
“I’m 34 in a few months,” she says wryly, “and I’m on hectic medication which I’m extremely thankful for but which has brought on early menopause. I have scars all over my body, I’ve had six operations to try to reconstruct my breasts and my body image has taken a serious beating. Th is is when I’m supposed to be out there and at my sexual prime but I get hot fl ushes and my moods swing dramatically.
“Being in a committed, trusting relationship is the only way to go. Reassuringly there are amazing men out there – you just have to fi nd the right one. “At times it’s diffi cult not to feel sorry for myself but on the other hand I also feel I have to be strong and upbeat for the people closest to me.”
Wilma: "This worked for me"
Wilma has several suggestions on how to best get through your cancer treatment.
“For starters you need to trust the team treating you,” she says. “You’re at your most vulnerable and you need all the support you can get. “I ‘m so grateful to the doctors and nurses who helped me. I appreciate the open and respectful way they dealt with all my questions and fears.
“On a more practical note, you really must get moving as soon as you can after a mastectomy. Wait for the physiotherapist to give you the all-clear, then do the exercises to keep your muscles from wasting away.
But don’t be tempted to drive too soon – you’d be surprised how exhausting it is.
“It’s also important to remember that everybody’s treatment and recovery are different so you shouldn’t compare yourself with other patients or you may end up feeling hopeless.
I never thought I’d bounce back but, although it takes time, you come through the experience and regain your energy and lust for life.”
Wilma's tips on managing chemotherapy:
- Sleep before you go in for chemo.
- Take your medication at the prescribed times.
- You might not feel too bad initially but be warned – it could hit you later.
- Eat healthily and make sure your diet includes plenty of fresh fruit and vegetables.
- Drink lots of water.
- Don’t plan anything for at least three days after the chemo. I always tried to have my chemotherapy on a Friday so I had the weekend to rest.
- Cut your hair really short when it begins to fall out otherwise it creates a real mess.
- Buy lots of stylish bandanas for your bare head so you can still make a fashion statement.
- Don’t go into the sun after you’ve had chemo as your skin will blemish easily.
- Your memory takes a beating and you won’t remember what happened yesterday. It’s a combination of many factors and it does improve so don’t worry.
Wilma's tips on managing radiation therapy:
- Rest well the day before you undergo radiation and try to have it first thing in the morning so you have the rest of the day ahead of you.
- Dust the area with Maizena beforehand.
- It seems to make the skin less sensitive.
- Wear loose shirts and no bra.
- Don’t have a warm bath or shower before or after sessions as this will irritate your skin.
- Don’t use creams or oils on the treated area. If your skin is very dry chat to your doctors about what you can use.
- Any burn marks will disappear slowly but surely.
- Ask the medical team to do the tattoo marker under your arm, not between your breasts where you’ll see it for the rest of your life.
- You’ll be tired so don’t plan a hectic weekend.
The latest on breast cancer:
More and more women under the age of 35 are getting breast cancer, according to the latest statistics. The reasons for the increase are unknown.
It’s more diffi cult to diagnose breast cancer in younger women than in older women. There are many reasons for this. One is that breast cancer is relatively rare in young women and therefore doctors might not suspect it during an initial visit.
The breast tissue is also fi rmer which makes it more diffi cult to detect a small lump. An ultrasound exam of the breast is the most reliable way to examine younger women because this method can detect a lump in fi rm tissue more easily. Nevertheless, in 10 per cent of cases a cancerous tumour will look like a fi brous adenoma (benign lump) on the screen.
That’s why it’s important to do an aspiration (fi ne needle biopsy) on all lumps. If it’s still not clear more tissue should be taken with a second and larger biopsy.
Strangely enough, most cases of breast cancer in women younger than 35 are detected during pregnancy or while they’re breastfeeding.
Some young women who have a strong family history of breast cancer consider having a double mastectomy as prevention. This may reduce the risk for these women and others with a high risk of developing breast cancer by as much as 90 per cent.
However, there is no absolute guarantee against breast cancer because breast tissue may also occur in the armpit, above the collarbone and in the abdominal cavity.
What to look out for:
The jury is still out on whether breast selfexaminations are a good enough means of detection.
Some doctors believe most women don’t know what they’re feeling for and recommend annual check-ups with their gynae or GP. But the Cancer Association of South Africa suggests you look out for:
- A change in the shape or size of the breast
- Dimpling, puckering or scaliness of the skin
- A lump or thickening in the breast or under the arm
- Discharge from one or both nipples
- Rash on the nipple
- Nipple retraction or scaliness
- A change in the colour or feel of the skin of the breast
- Change in skin texture such as “orange
peel” skin. If it is accompanied by swelling,
redness or a feeling of “heat” in the breast
it could be inflammatory breast cancer.
Around five per cent of young women with breast cancer get this aggressive form of cancer where no lump is felt.
Remember:
Nine out of 10 lumps are not cancerous. Seek an expert opinion for every new lump you find or if you notice a change.
Just because one lump was benign doesn’t mean the others will be too. Women older than 40 should go to a gynaecologist or oncologist for a detailed breast examination once a year.
A mammogram or ultrasound should be done every two years.
Breastfeed for as long as possible if you’ve had a baby.
Live healthily and drink in moderation.
Who is at risk?
According to the 1998-1999 National Cancer Registry one in 12 white women has a risk of developing breast cancer.
In Asian and coloured women the risk is one in 18. Black women have the lowest incidence rate of all population groups: one in 49.
What the doctor says:
“Cancer survivors live with the disease every day,” Dr Irene Boeddinghaus, oncologist at the University of Cape Town’s private academic hospital, says.
“Some cases are cured but you only ever know that in retrospect. And unfortunately there is no convenient way of picking up whether the cancer has recurred.
With prostate cancer, for instance, there is an easy blood test which doctors can do regularly to check if there is a recurrence but there’s nothing that’s anywhere as good as this for breast cancer.
“You might go home from surgery and/or treatment but then you face the really hard task of getting your head around the fact that you don’t know if you’re cured or not. I encourage women to live and act as if they are cured but you do need to have regular check-ups. Over time the recurrence rate goes down but it’s never zero.
You can probably consider yourself cured after 10 years but you’ll need to have an annual mammogram for the rest of your life.
“Because there is no cure for breast cancer the next best step is prevention. One of the best things you can do is breastfeed for as long as possible if you’ve had a baby but sadly employers don’t usually like this too much.
Also becoming pregnant before 30 is helpful. Until you have completed a full term of pregnancy your breast cells sit in a state of suspended animation and this is when maverick cells can begin changing. Pregnancy puts breast cells in the fi nal stage of development and this is what needs to happen for them to remain healthy.
“Cancer does seem to be linked to lifestyle but there are no hard-andfast rules you can follow to ensure you don’t get the disease. Every woman is different and you can’t over-simplify.
“The occurence of breast cancer in North America and Western Europe is six to 10 times greater than in Japan, Asia and Africa. In South Africa white women are more vulnerable than other population groups but the incidence in young black women is picking up too, presumably as they adopt an urban lifestyle.
“Genetics have a role to play but so do other factors such as breastfeeding practices, family size, stress and types of contraception. But something you can control is your intake of alcohol and your weight. Alcohol inhibits the functioning of your liver which metabolises oestrogen. We know that raised levels of this hormone appear to make women more vulnerable to breast cancer.
Losing weight post-menopause is also recommended.”
Dr Boeddinghaus says for all the anxiety around the disease there are enormously exciting new drug developments.
“There used to be only a blunderbuss approach where doctors blasted patients with really high doses of chemotherapy in the hope it would have some impact on the mutant cells.
Some of the drugs were seriously toxic and it’s no wonder people often felt really terrible. But today there’s much more subtle, targeted molecular therapy which in some cases is the longed-for silver bullet. These new-generation drugs offer patients light at the end of the tunnel.
“Developments in plastic surgery are also heartening. You can go in for a mastectomy, for instance, and wake up with a reconstructed breast.”
Risk factors and breast cancer
– what’s important?
We know certain factors are implicated in breast cancer. The disease is a hundredfold higher in women than in men. It most often develops in older women (85 per cent of cases present in women older than 50).
The third most important factor is a family history in which at least two close relatives (your mother or sister) developed breast cancer before the onset of menopause. This doubles your risk. If one close relative has breast cancer your chance of getting it too is one in five.
Cancer in the other breast, previous biopsies showing abnormal or unusual growth of breast tissue and radiation therapy in the chest area for other types of cancer, can also increase your risk for breast cancer.
Then there’s the link between breast cancer and oestrogen. Anything that increases and prolongs your exposure to this hormone increases the likelihood of your developing breast cancer.
That includes: early menstruation and late menopause, the use of hormone replacement therapy (HRT) for five years or more, and a first pregnancy after 30.
The fewer pregnancies you have and the shorter the period for which you breastfeed your baby, the higher your breast cancer risk. What’s more, regular alcohol consumption (one or more drinks a day) increases a woman’s risk, as does being overweight after menopause.
Did you know?
A woman’s chances of surviving breast cancer depend largely on the surgery and the skill of the surgeon. Get a second opinion if you’re unsure.
Mammograms are safe. An experienced radiologist can detect a lump of 0,5 – 1 cm while self-examination allows you to detect only a lump of 2 cm in diameter.
If you have cancer in one breast you run a risk of getting it in the other breast as well.
Your chances of getting breast cancer are only slightly higher than normal if you previously had benign lumps in your breast.
A type of breast cancer called ductal cancer in situ (DCIS) has an excellent recovery rate if it is detected at an early stage.
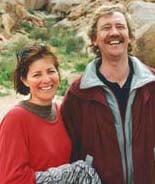
THE ROAD TO RECOVERY. Melléta Louw in January 2003 with her husband, Kobus, shortly before she felt a small lump in her breast. By September she was halfway through her chemotherapy, having lost 7 kg – and her hair. December 2003 in Stilbaai, just after her treatment ended.
GET YOUR TEST
FOR LESS
As she did last year, Wilma
has arranged a special
discount of 10 per cent
for mammograms at radiologists
countrywide. This
offer is valid throughout
October which is Breast
Cancer Month. Visit www.health24.com
to see which radiologist near you is
taking part in this special offer.
For more information on breast cancer or for details of your nearest Reach for Recovery support group call Cansa toll-free on 0800-22-66-22, e-mail info@cansa.org.za or visit www.cansa.org.za
For more information on breast cancer and treatment visit our breast condition centre
This story originally appeared in the first edition of Pulse magazine. Buy the latest copy, on newsstand now, for more fascinating stories in the world of health and wellness.




 Publications
Publications
 Partners
Partners