Blink. Blink. Blink. His eyes were the only thing that could move as Charles Oppelt lay in pain on the green grass on a sunny Saturday afternoon, waiting for help.
When help came, the 17-year-old Oppelt waited further – he waited and waited and waited and waited. He waited more than 14 hours before receiving treatment for a rugby injury that left him permanently paralysed.
However, the wait was not yet over.
Everything changed in minutes
He waited another decade seeking compensation from the Western Cape health department for failing to promptly conduct a procedure that could have prevented his spinal injuries from leaving him disabled from the neck down.
Oppelt comes from Atlantis, Cape Town, and had big dreams of being an outstanding rugby player. However, when he took to the field as a hooker for Mamre Rugby Club's third team on March 23, 2002, it was only minutes before everything changed.
His head rammed into an opponent's shoulder when a scrum collapsed, causing a severe injury to his cervical spine.
"I was scared. My body was so weak and I felt so uncomfortable," Oppelt told Health24 recalling the events. He was also in pain, but words failed him: "It was a pain I can't put into words."
As he lay on the grass, he could not move a single limb beyond his eyes. "I couldn't move. I couldn't even lift my hands. There was no movement in my whole body. The only thing I could move was my eyes."
As if he knew what was to come, Oppelt felt paralysed, his body resembling a corpse.
"To me it was like a body on the ground, just moving his eyes. It felt like my legs were under my back and my feet by my head. It did not feel like I was going home ... it was like I was going to the cemetery."
Oppelt was taken to a nearby hospital by ambulance before being taken to Groote Schuur Hospital where he had to wait for hours before receiving attention. The following morning he was taken to Conradie Hospital, where he underwent an operation.
While being transported between hospitals, Oppelt wondered what was happening – but he remained certain that his injury would change his life.
"I realised this [accident] was something very dangerous."
'Mummy, where are my legs?'
He spent a year recovering in Conradie Hospital where his mom Helen Oppelt faced her most difficult moment as a parent.
"One morning, when I came to the hospital and Charles asked me 'Mummy, where are my legs?'" It prompted her to ask her own question: "How do I as a parent tell my son he will not walk again?"
Helen could not utter those words out loud so she searched out his doctor. "That morning the wards at Conradie Hospital were not big enough for me to run through as I tried to get Charles answers."
As his mother recalled this moment, a sea of sorrow rose in Oppelt’s eyes. As quickly as a tear rolled down his right cheek, he wiped it away.
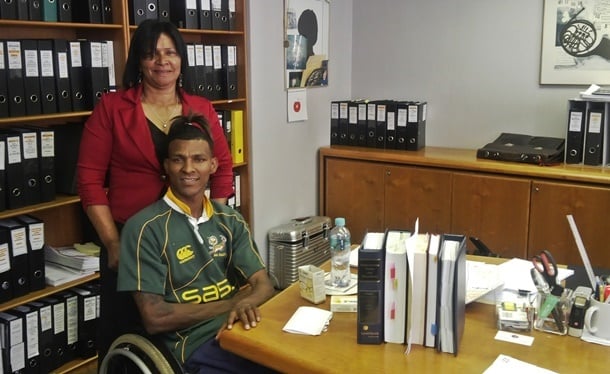
Image: Charles Oppelt with his mother Helen. (Adiel Ismail)
He had initially found it hard to accept what had happened, but during rehabilitation learnt how to deal with his paralysis.
"I was a hyperactive person and always on the run. It was really hard for me. I had to wait for someone every time to help me. If I wanted to go to the shop or visit my friends, a caretaker had to help me."
The worst was yet to come.
"There were times when I was so depressed I didn’t want anyone around. I would just sit in my bedroom and, when someone would come around, I was an angry person.
"I thought there was nothing for me to live for. When looking through the window, I would see people playing rugby or my own friends would visit me with a rugby ball and I would ask myself why I must sit in this wheelchair. I had a lot of questions as I reached the bottom in my life. Sometimes I would tell God: ‘You can just come take me, because what is the reason for me to live.'"
Another challenge has been the 13-year protracted legal case against the health department. Throughout that difficult legal process, Oppelt had to regularly return to court and explain the process that had led to his injuries – opening up the wounds yet again.
"My life was on hold for 13 years because of this case."
Following legal wrangling, the Cape High Court ruled in November 2012 the provincial health department should compensate Oppelt. However, this judgment was overturned when the department appealed to the Supreme Court of Appeals.
Watch: Oppelt's attorney Hans-Peter Scheibert explains to News24Live the dynamics of the case and what this victory means.
Closed cervical reduction
Thereafter, Oppelt turned to the Constitutional Court (Concourt). The highest court in the land ruled in October this year the Western Cape Health Department had been negligent in its treatment of him, finding his paralysis could have been avoided.
At the heart of these legal arguments was a procedure called closed cervical reduction. This technique involved stretching the spine to release pressure on the spinal cord and encourage blood flow – and prevents tissue dying off.
However, Dr Dennis Newton, the orthopaedic surgeon in charge of the Conradie Spinal Cord Injuries Unit, argued in court the procedure had to be performed within four hours of the injury. Court papers indicated:
14:15 – Oppelt suffered his injury.
15:15 – He arrived at Wesfleur Hospital and was attended to by a nurse and a doctor.
16:00 – The doctor phoned the training neurosurgical registrar at Groot Schuur Hospital. He suggested Oppelt be transported by helicopter to Groot Schuur, a call that would have taken 12 minutes had it materialised.
16:55 – Oppelt is transported from Wesfleur by ambulance.
17:40 – He arrives at Groote Schuur.
18:00 – The training neurosurgical registrar examines Oppelt.
20:22 – An Orthopaedic surgery registrar calls the ambulance for an urgent transfer to the Conradie Hospital specialised spinal cord injury unit.
00:25 – Ambulance is dispatched only on the morning of March 24, 2002.
01:08 – Ambulance departs from Groot Schuur.
01:23 – Ambulance arrives at Conradie.
03:50 – Closed reduction procedure takes place.
The basis for Dr Newton's four-hour cut-off theory was that neurological cells deprived of glucose and oxygen for more than four hours could not be brought back to life. However, the department argued there was no consensus in the medical field on this.
Spinal surgeon Nicholas Anthony Kruger told Health24 the application of cervical traction reduction remained controversial with many clinicians believing it remained a specialist procedure.
"This perception is incorrect and if one had to critically audit it, I am sure most neurosurgeons and orthopaedic surgeons would feel uncomfortable performing a cervical reduction unless they had a largely spinal surgery based area of expertise," he said.
'A reduction can be done in 30 minutes'
"The main problem is a patient is sent to the nearest hospital for treatment, but the doctors there are unable or unwilling to perform the cervical reduction. This results in delays from ambulance transfers to alternative hospitals and inevitable delays in the cord decompression."
Kruger noted most animal models and human outcome studies suggested the more rapid the decompression, the better the final neurological outcome.
"That is why I feel the primary hospital needs to be able to reduce the dislocated neck when indicated and not wait for several hours to transfer the patient. A reduction can be done in 30 minutes once diagnosed and the cord given the best chance of recovering some function."
Kruger said the probability of making a patient permanently worse during cervical reduction was less than 1% with a transient neurological deficit risk of about 1-4%. About 80% of cervical reductions were successful, making them "a remarkably safe procedure".
He advocated for a change in medical perceptions about the reduction of cervical dislocations.
"Ideally every cervical dislocation would have a competent specialist immediately available to perform the reduction. However, this is not practical and in reality specialists may be busy operating, off site or not comfortable with the reduction," said Kruger.
Patients with cervical dislocations and severe neurological deficits or rapidly deteriorating neurological levels, had nothing to lose and everything to gain, he said.
Kruger said a proper examination and simple X-ray diagnosed the problem and urgent cervical reduction needs performed by a trained primary hospital emergency doctor when the resident specialist was not immediately available.
An extra hour or two delay
"There is no need to delay indirect cord decompression by waiting for a specialist to arrive and there is no need for an MRI in this scenario. The basic equipment needs to be standard in every district level hospital and above."
He said some doctors felt an MRI scan was required before a reduction and argued to transfer patients to facilities where this could be done.
"I am also not in agreement with this. Many studies have shown MRI scans do not show any clinically useful information about a dislocated neck; they may instead change the doctor’s management and perception about the safety of cervical reduction and impose risk due to moving an unstable neck in and out the scanner, as well as causing an extra hour or two delay in treatment."
Hoping to change the medical perceptions about cervical reductions, Kruger said he recently conducted a survey of cervical traction in the Western Cape.
He found most doctors had no formal training; thought it was a dangerous procedure to the patient and preferred to transfer or refer the patient away rather than intervene and save a dying cord.
"Most district level hospitals did not even have the basic equipment available even though it is on the World Health Organisation (WHO) recommended essential equipment list for district hospitals," he said.
Rugby injuries with cervical dislocations were probably the one group that stood to benefit most significantly from urgent cervical reductions, Kruger said.
"They are young patients with good biology and are low energy-type injuries, which have a better prognosis than higher energy injuries such as motor car injuries or falls from heights."
The department told Health24 it respected the Concourt judgment, but was seeking senior legal opinion on matter.
"We are concerned by the judgment and the impact it could have on health care provision going forward," health department spokesperson Mark van der Heever said.
Oppelt’s compensation has yet to be determined, but was expected to run into millions.
"Charles may have won the case and, while it will improve his life, it cannot buy him legs," his mother said.
Reflecting on this accident, Oppelt said: "If I look back now, I can still feel the pain."
After a long pause, he continued: "But I am a stronger man. I am very grateful I am breathing today."
Blink. Blink. Blink. His eyes bright with the rays of life, Oppelt now plays wheelchair rugby for Stellenbosch University, where he will study sports science being the sports fanatic he is.
Watch: Oppelt speaks to News24Live about his accident.
Also read:
New rugby scrum technique may be safer
Injuries to lower limbs common in rugby
How a physiotherapist would manage a dislocated shoulder or knee




 Publications
Publications
 Partners
Partners