Introduction
About 20% of the population get a migraine headache sometime in their life – that means over a billion people worldwide at some point get migraines. This percentage has been shown to be constant across races, cultures and income groups. Migraine does not discriminate. In SA, a country of 49 million people this equates to about 9 million migraineurs. It is estimated that 25 million working days are lost each year due to migraine. Due to this many migraineurs fear losing their jobs because of their condition – and for some this becomes a reality.
Definition
This is the most common type of vascular (from blood vessels) headache. Migraine headaches can be divided into two main types:
- Migraine with aura (previously known as classic migraine)
- Migraine without aura (previously known as common migraine)
From 20-30% of migraines occur with an aura, which is a collection of symptoms that usually occurs 15 to 30 minutes before a migraine headache begins. The most common aura symptoms are visual disturbances, such as flashing lights, distortion in the size or shape of objects (zigzagging), or blind or dark spots in your field of vision. An aura may also include other symptoms affecting your nervous system, such as numbness or tingling in your face or arm, strange smells or sounds, difficulty speaking, or weakness on one side of your body.
Sex differences
Women suffer more often from migraines than men, in fact, 18% of women get migraines in comparison to only 6 % of men. This is due to the effects of estrogen, a female sex hormone which is very important in regulating the menstrual cycle. Estrogen also helps the brain cope with pain, so a drop in estrogen means that the brain registers pain more easily. The important changes in estrogen levels occur just before menstruation begins. Oral contraceptive pills and hormone replacement therapy during menopause also affect oestrogen levels. During pregnancy, particularly during the last 6 months, oestrogen levels rise, and most migraine sufferers have fewer attacks during this period.
Age differences
Before puberty, an equal number of boys and girls get migraines. But during and after puberty, migraines affect girls three times more often than boys. Thispattern continues even after menopause. Migraine attacks start before the age of 20 in a majority of cases. According to one study, the peak age of onset migraine for females was at 14-17.
Genetics
Migraines do have a hereditary component. Experts have shown that the likelihood of getting migraines is inherited. If one of your parents gets migraines, you have a greater chance of having these types of headaches than someone who doesn't have a family history of migraines.Migraines are passed from parent to child, because we pass on muscle structure, general posture, and internal anatomy of arteries and nerves much the same way as we pass on height, build, and looks. That migraine has a genetic component doesn’t affect treatment however – in other words, it can still be successfully treated even if it is inherited.
Causes
Although scientists have yet to determine the cause of migraine, we do know where the pain comes from. Most migraine pain originates in the arteries of the scalp or from the jaw and neck muscles. When the muscles become tense, the arteries can become painful. Although migraine has an arterial component to the pain, it can often be prevented by treating the tension in the jaw and neck muscles. When the muscles relax, the arterial pain often subsides as well. The arteries involved in migraine are usually the superficial temporal arteries (on the temple) or the occipital arteries (at the back of the head). In rare cases other small arteries in the scalp may also be involved.
Migraine triggers
One of the most confusing things about migraine is that it can be triggered by many different things. The result is that, understandably, people think the trigger is what caused the migraine. The million dollar question, though, is why does a particular trigger, like chocolate, for example, trigger migraine in one person and not in another? The answer is that in the migraine sufferer there is an underlying problem which is made worse by a chemical in the chocolate, thus triggering an attack. The real problem is the underlying problem – once this is identified and treated, the ‘trigger’ no longer causes an attack.
You will be able to find out if you have a particular trigger for your migraines by keeping a migraine diary. Each time you suffer from a migraine, make a note about the warning signs, triggers and severity. If you can discover some of your personal triggers, you may be able to avoid future migraines. This diary is important as it will give your medical professional an accurate history of your migraines. A migraine diary is available free of charge at www.headacheclinic.co.za under Free Assistance.
Common triggers
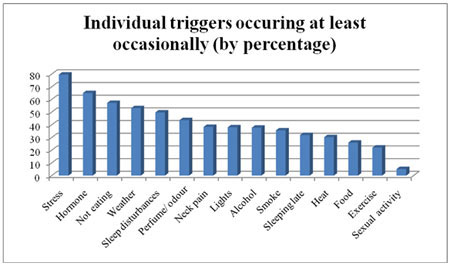
In a study published in Cephalalgia, The International Journal for Headache, one thousand two hundred and seven migraine patients were tested at The Headache Centre of Atlanta, a clinical practice in the USA. The graph below shows the results of this study:
Symptoms
The pain of a migraine is felt as an intense, throbbing pain in the forehead, temple, ear, jaw or even around the eye. It usually starts on one side of the head, but eventually spreads to the other side. It is sometimes preceded by an aura. The aura is usually visual disturbances like zigzag lines or a temporary partial loss of vision, but may also include numbness of the lips and arm, and difficulty in speaking. The migraine is often accompanied by other symptoms such as nausea, vomiting, sensitivity to light, and sensitivity to noise. An attack usually lasts from 4 to 72 hours – averaging 12 to 18 hours – and may be incapacitating enough to disrupt daily activities.
Course
During the initial stage of a migraine, the nervous system reacts to a trigger, and causes a spasm in the arteries at the base of the brain, which are rich in nerves. The spasm constricts several arteries which supply blood to the brain and reduces its blood flow. This causes the aura. As the aura subsides, the pain usually starts. The pain may come from one of two structures – the arteries in the scalp, or the muscles of the jaw and neck.
Diagnosis
The history and physical exam are all that is needed to diagnose migraine headaches. Additional tests are only needed to help diagnose other conditions which may cause similar symptoms. See Diagnosis under Headaches. Brain scans are not necessary unless the initial neurological examination suggests that one should be done.
Treatment
Migraine treatment is often with medication, but most migraine sufferers respond very well to non-drug treatment.
Medication
Two types of drugs are used:
- Medication to treat an attack
- Medication to prevent an attack
Medication to treat an attack
In some people, migraine headaches can be relieved by a mild painkiller - for example, paracetamol, aspirin or naproxen (NSAID) - if taken in high enough doses and if taken early enough at the time of an attack. Stronger analgesics, containing codeine or caffeine, are often necessary. If nausea or vomiting accompany the migraine, tablets may not be absorbed sufficiently from the gut. Effervescent tablets or suppositories are then often more effective.
Anti-nausea medication can help to reduce accompanying nausea and vomiting.
Ergot alkaloids (made from a fungus that grows on grain), such as Cafergot or Migril, might help if taken early enough, but are not effective once the headache is established. In excess, especially with poor timing, these medications may exacerbate rather than alleviate a headache. Ergotamine has a number of side-effects. Care should be taken not to exceed the recommended dose.
The triptan drugs, Imigran, Maxalt, Relpax, Zomog, Axert, are effective in many cases. The medication is available on prescription and can be used at any stage of a migraine – bringing rapid relief in about half an hour in approximately 80% of patients.
The triptans, Cafergot, and Migril all have the same mode of action – they constrict the painfully dilated and stretched arteries in the scalp. If they are effective, then it means that the pain originates in the scalp arteries. In these patients, surgical treatment of these scalp arteries is a permanent solution to the problem.
Medication Overuse Headache
The biggest problem with the ‘rescue’ medications is that if they are taken on a regular basis, they may cause a condition called Medication Overuse Headache (MOH). This means that the drugs themselves gradually cause the headaches to get worse, more severe, and more frequent. The patient then has to increase the dose, and a vicious cycle of worsening headaches and increasing amounts of drugs is set up. His is why the non-drug approach is preferable.
Medication to prevent an attack
If attacks occur more often than three times a month, drugs to prevent attacks are often prescribed. The drugs commonly used to prevent migraine are not often effective, though, and frequently cause such unpleasant side effects that patients stop taking them and prefer to live with the pain instead.
Drugs to prevent migraine include
- Beta-blockers, such as propranolol (i.e. Inderal) – which will reduce blood vessel dilatation
- Pizotifen (Sandomigran) – unfortunately often associated with weight gain
- Anti-epileptic drugs
- Anti-depressants, such as amitriptyline
- Clonidine – which inhibits blood vessel contraction and dilatation
- Flunarizine (Sibelium) methysergide
- Cyproheptadine (Periactin)
Non-drug treatment
Most patients, given the option, opt for non-drug treatment.
The first step in non-drug treatment is to diagnose where the pain is actually coming from. In Migraine there are two anatomical structures where the pain most often starts. It may come from:
- The muscles of the jaw and neck
- The arteries of the scalp (not from inside the brain)
Muscle pain
The best treatment for the muscle component of migraine pain is by means of a plate worn in the palate, called a Posture Modifying Appliance or PMA. Wearing the PMA causes the jaw and neck muscles to relax, and is effective in many migraine sufferers. In 5 out of six cases, this is all that is necessary. Other treatments such as physiotherapy, exercise, traction, Botox, and minimally invasive bloodless surgery are also used for the muscle tension component.
Artery pain
It is interesting that in many patients with artery pain, when the muscles are relaxed by means of the PMA, the artery pain also subsides. In those patients where the pain doesn’t improve with the PMA, the arteries can be treated surgically. In many migraine sufferers this is a permanent cure for their migraines.
Previously reviewed by Dr Andrew Rose-Innes, MD, Department of Neurology, Yale University School of Medicine, New Haven
Reviewed by Dr E. Shevel, BDS, Dip MFOS, MB, BCh, Maxillo-facial and Oral Surgeon, Medical Director, The Headache Clinic, Johannesburg, Durban, Cape Town, August 2011




 Publications
Publications
 Partners
Partners