The purpose of pre-test HIV counselling is to provide you with information on the technical aspects of testing and the possible personal, medical, social, psychological, legal and ethical implications of being diagnosed as either HIV positive or HIV negative.
The purpose of pre-test HIV counselling is further to find out why you want to be tested, the nature and extent of your previous and present high-risk behaviour, and the steps that need to be taken to prevent you from becoming infected or from transmitting HIV infection.
The counsellor will usually follow the following guidelines in pre-test counselling:
1. Reasons for testing
The counsellor will explore the reasons why you want to be tested:
Is it for insurance purposes, because of anxiety about lifestyle, or because you have been forced by somebody else to take the test? What particular behaviour or symptoms are causing concern to you? Have you been tested before, and, if so, when? For what reason? And with what result?
These questions provide the counsellor with an opportunity to ascertain your perceptions of your own high-risk behaviour, and with allows you to assess whether you intend to be tested and whether your fears are realistic or if you are unnecessarily concerned. The following are some of the reasons that clients who want to be tested often give:
- Their partner has requested it.
- They want to determine their HIV status before starting a new relationship.
- They want to be tested prior to being married.
- They feel guilty and concerned about having multiple sex partners.
- They have had recent sexual encounters in which they did not use condoms.
- They are manifesting symptoms that are giving them cause for concern.
- They are been referred by a STI or TB clinic because the client has tuberculosis or a sexually transmitted infection.
- They have come to re-confirm a positive HIV test.
- Their current partner is HIV positive, or they were once involved with a partner who was HIV positive.
- They plan to become pregnant and want to check their HIV status before they do so.
- They have been raped or assaulted.
- They need to be tested after an occupational exposure (e.g. a needlestick).
- There are simply curious.
The reason why a client wants to be tested is important because it sets the scene for the rest of the pre-test counselling session.
2. Assessment of risk
The counsellor will assess the likelihood of whether you have been exposed to HIV by considering how much and how frequently you have been exposed to the following risk factors and lifestyle indicators:
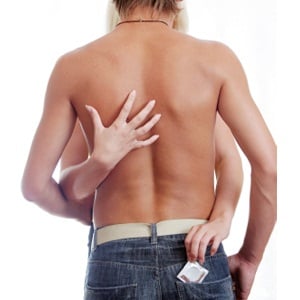
- What is your sexual risk history in terms of frequency and type of sexual behaviour? Have you been involved in high-risk sexual practices such as vaginal or anal intercourse with more than one sex partner without the use of condoms? In the case of anal sex, was it anal-receptive or anal-insertive sex? Did you have sex with a sex worker (or prostitute) without a condom? Or is your sex partner HIV positive?
- Are there any other risks involved? Are you an intravenous drug user, a prisoner who is exposed to rape or unprotected sex in prison, a migrant worker, a refugee or a sex worker? Have you been raped or coerced to have sex with another person? Do you have another sexually transmitted infection or tuberculosis?
- Did you receive a blood transfusion or body products in a developing country where testing blood for HIV is not standard practice? Note: All blood supplies in South Africa are tested for HIV, and are very safe.
- Have you been exposed to possibly non-sterile invasive procedures such as tattooing, piercing or traditional invasive procedures such as male or female circumcision and scarification for the application of medicines?
- Have you been exposed to HIV-infected blood in the work situation? (E.g. injuries with large volumes of blood involved, or needlestick injuries.)
3. Beliefs and knowledge about HIV infection and safer sex
- The counsellor will determine exactly what you believe and know about HIV infection and Aids and he or she will correct errors or myths by providing accurate information about transmission and prevention.
- The counsellor may also ask you about your past and present sexual behaviour and provide information about safer sex practices and a healthier lifestyle. He or she should find out if you know how to practise safer sex and how to use a condom correctly. They will also supply you with condoms. Sex is natural and nothing to be ashamed of. Allow the counsellor to ask these questions, because that is the only way he or she can give you empowering information to enjoy sex safely.
4. Information about the test
The counsellor will ensure that you know exactly what the HIV test entails. The counsellor will explain the following points to you, and if he or she does not, you now know what questions to ask:
- There is a difference between being sero-positive and having Aids. The HIV antibody test is not a “test for Aids”. It indicates that a person has HIV antibodies in the blood and that the person is infected with HIV. It does not say when or how the infection occurred, or in what phase of infection the person is.
- The presence of HIV antibodies in the blood does not mean that the person is now immune to HIV. It means that he or she has been infected with HIV and that he or she can pass the virus on to others.
- The meaning of a positive and a negative test results.
- The meaning of the concept of the “window period”. The need for further testing will be emphasised if the person practises high-risk sexual behaviour and tests negative.
- The reliability of the testing procedures. A positive HIV antibody test result is always confirmed with a second test and the reliability of test results is usually high. False-positive or false-negative results may, however, occasionally occur despite the general reliability of HIV tests (e.g. a false negative test result because the person is in the window period).
- The testing procedure. Many clinics in South Africa use HIV antibody rapid tests, which means that the finger will be pricked to get a drop of blood. The results are available within 15 to 30 minutes. The counsellor will explain how blood is drawn for the Elisa test (if rapid testing is not available), where it is sent (if a rapid test is not used), when the results will be available and how the person will be informed of the outcome.
5. The implications of an HIV test result
The counsellor will discuss the possible personal, medical, social, psychological, ethical and legal implications of a positive test result with you prior to testing. He/she will inform you about all the advantages and disadvantages of testing. The following advantages can accrue from taking the test:
- Knowing the result may reduce the stress associated with uncertainty.
- One may begin to make rational plans for preparing oneself emotionally and spiritually to live with HIV.
- Symptoms can be confirmed, alleviated or treated.
- Prophylactic (preventative) treatment can be considered, for example for tuberculosis.
- Anti-retroviral treatment can be considered.
- Adjustments to one’s lifestyle and sex life can protect oneself and one's sex partners from infection.
- One can make decisions about family planning and new sexual relationships.
- One can plan for future care of one’s children.
The disadvantages that might accrue from taking an HIV test (especially if its result is positive) include:
- Possible limitations on life insurance and mortgages.
- Having to endure the social stigma associated with the disease.
- Possible problems in maintaining relationships and in making new friends.
- A possible refusal on the part of uninformed medical and dental personnel to treat an HIV-positive person. (A refusal to treat HIV-infected individuals of course goes against the provisions of the South African Constitution.)
- Possible dismissal from work (although it is illegal to dismiss people because they are HIV-positive).
- Possible rejection and discrimination by friends, family and colleagues.
- Emotional problems and a disintegration of one’s life.
- Increased stress levels and uncertainty about the future.
- The stress and negative effects of maintaining a secret if the person decides not to disclose his or her test results.
- How would you feel if you tested negative? How would you feel if the test were to be negative but you were advised to be tested again because you may still be in the window period?
- What would your reactions and feelings be to a positive test? Would a positive test change your life? How? What negative changes would you anticipate? What positive changes can you imagine?
- Do you intend to tell others if you test positive? Who would you tell? Why that person? How would you tell them? Why would you tell them? Clients must be warned about people’s possible reactions. Often those closest to the client cannot cope with such news. The counsellor must help clients to think not only of themselves but also of those who are to be told. (For example, if the client says to you: “The news will surely kill my old and frail mother”, you may ask: “Why do you want your mother to know?”). Clients must also be warned that some people may not keep the information to themselves, and that this might have harmful effects for the client.
- How would you tell your sexual partner? If the test result is positive, the sexual partner also needs to be tested.
- How would a positive test result change the circumstances of your job, your family and your relationships? Would your relationships be improved or hindered by telling people you were HIV positive? What do you believe their reactions would be?
- Where would you seek medical help? How do you feel about a disease that requires a lot of care, lifestyle changes, commitment and discipline? Do you have members of your family or friends who could help you to be disciplined about your health? Could you take medication every four hours if necessary?
- Who could provide (and is currently providing) emotional and social support (family, friends, others)?
- Find out the names of people whom the client might contact for moral support while he or she waits for the results.
- Encourage the client to contact you or a colleague if they have any questions.
- Counsel the client on how to protect sex partners (e.g. to use condoms) in the waiting period.
- Encourage the client to do something enjoyable to keep himself or herself occupied while waiting for the results (e.g. hiking, going to the movies or playing soccer with friends).
The counsellor will tell you about medical treatments that are available which can help to keep you healthier for longer.
6. Anticipate the results
It is important to anticipate a positive HIV antibody result and to talk about how the client will deal with a positive test outcome. Anticipating a positive result helps the counsellor to ascertain the client's ability to deal with, and adjust to, a positive result. The counsellor also gains insight into some of the potential problems associated with a positive test outcome.
Preparation for the possibility of a positive test result, paves the way for more effective post-test counselling. In order to prepare you as client for the test result, the counsellor should ask the following questions:
The choice to be tested remains the client’s prerogative. The advantages of testing can be explained to clients, but clients should not be forced to be tested if they feel that they will not be able to deal with the results. The mere knowledge of people’s HIV status will not necessarily protect them, or their loved ones, from infection.
People who prefer not to be tested should, however, live as if they are infected and practise safer sex at all times. People who suspect they are HIV infected should also refrain from donating blood.
7. Confidentiality of test results
The counsellor should stress the confidentiality of test results. The client’s right to confidentiality must be respected at all times. If individuals choose to remain anonymous, they must be reassured that no information will be communicated without their prior permission to anyone.
The client’s consent must be obtained before anyone can pass on any information about his or her HIV status to any other health care professional who also treats the client. If the counsellor explains why other health care professionals need to know about the client's HIV status, most clients will consent to this information being given out.
8. Informed consent
The decision to be tested can only be made by the client and their informed consent must be obtained prior to testing. Consenting to medical testing or treatment has two elements: information and permission. Before an HIV test can be done, the client must understand the nature of the test, and he/she must also give verbal or written permission to be tested. A client may never be misled or deceived into consenting to an HIV test.
Note to health care professionals: According to the law, health care professionals may not do an HIV test on a person unless he or she clearly understands what the purpose of the test is, what advantages or disadvantages testing may hold for him or her as client, why the health care professional wants this information, what influence the result of such a test will have on his or her treatment, and how his or her medical protocol will be altered by this information.
9. Information about giving the results and ongoing support
The counsellor will explain to you when, how and by whom the results of the test will be given. The counsellor will assure you of personal attention, privacy, confidentiality and ongoing support and advice if needed.
10. The waiting period
Waiting for the results of an HIV antibody test can be an extremely stressful period for the client. This waiting period (in cases where the rapid HIV antibody test is not being used) can last from two to 14 days, depending on where the test was done (whether by a private practice, a governmental health service or a rural clinic).
The results of rapid HIV antibody tests are, of course, available within 30 minutes. However, if the client has to wait for the test results, the counsellor should anticipate this difficult waiting period by discussing the following points with the client:
Note to counsellors: Pre-HIV test counselling is extremely important. It should not only be seen as a preparation for the HIV test, but as a golden opportunity to educate people about HIV/Aids and safer sex. Remember that this may be the one and only time that you will see the client because he or she might decide not to be tested, or not to come back for the test results after all.




 Publications
Publications
 Partners
Partners














