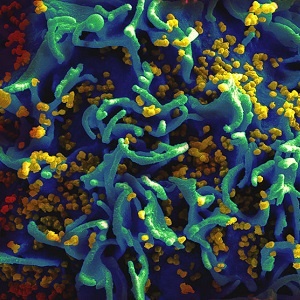
Highly active anti-retroviral therapy (HAART) has helped millions survive the human immunodeficiency virus (HIV). Unfortunately, HIV has a built-in survival mechanism, creating reservoirs of latent, inactive virus that are invisible to both HAART and the immune system.
But now, researchers at UC Davis have identified a compound that activates latent HIV, offering the tantalizing possibility that the virus can be flushed out of the silent reservoirs and fully cured. Even better, the compound (PEP005) is already approved by the FDA. The study was published in the journal PLOS Pathogens.
"We are excited to have identified an outstanding candidate for HIV reactivation and eradication that is already approved and is being used in patients," said lead author Satya Dandekar, who chairs the Department of Medical Microbiology and Immunology. "This molecule has great potential to advance into translational and clinical studies."
While HAART has been quite successful - reducing HIV infection in newborns, restoring patients' immune systems and lowering viral loads to virtually undetectable levels - these therapies cannot cure the disease alone. Once treatment is discontinued, pools of latent virus reactivate, and the infection comes roaring back. As a result, patients must remain on treatment indefinitely, posing the risk of long-term toxicity.
"We've made great progress, but at the end of the day you still have more than 30 million people walking around with HIV," said Dandekar. "Without drugs, the virus can come back at the same threat level for patients. Eradicating HIV is extremely critical."
Read: Results from two major trials may revolutionise how HIV is treated
'Shock and kill' approach
Eradication means activating latent virus and destroying it, a strategy called "shock and kill." Researchers around the world have been working on this approach, but finding the right compounds has been challenging. A successful molecule must precisely target proteins associated with HIV latency without overstimulating the immune system or wantonly activating protein master switches, such as NF-kappaB. Either outcome can generate severe side effects.
The UC Davis team may have succeeded with PEP005, the active ingredient in the FDA-approved anti-cancer drug PICATO, which increased HIV activation in patient blood samples and showed low toxicity.
However, HIV is a complicated virus and, as clinicians have discovered with HAART, must be treated through multiple means. In addition to PEP005, the researchers tested other compounds capable of reactivating HIV through different pathways. This painstaking process identified another molecule, JQ1, which works synergistically with PEP005 to maximize HIV activation. PEP005 when combined with JQ1 increased HIV activation up to 15-fold.
While these results are promising, researchers are mindful that "shock" only works when it's followed by "kill."
"First, we need to identify the best combination of latency-activating agents," said Dandekar. "Then we must help patients clear these reactivated cells. Just reactivating the HIV from latency won't be enough."
Dandekar notes that many HIV patients receiving HAART regimens have robust immune responses, which will go a long way towards clearing the virus. She also believes HIV vaccines in development could give patients an extra edge. Even a vaccine that isn't 100 percent effective at preventing transmission could boost a patient's ability to destroy reactivated virus.
However, identifying PEP005 and JQ1 as potent HIV-activators is a key step in the right direction.
"It is really exciting is that the molecule in PICATO is already approved and being used by patients," said Dandekar. "In addition to being very effective in reactivating HIV, it also works beautifully with other latency reactivating agents, is less cytotoxic and doesn't cause a major immune response."
Read more:
Teen's HIV in check 12 years after stopping ARV's
The sooner you start ARV's the better
Its time to override patents on HIV drugs




 Publications
Publications
 Partners
Partners














