Definition
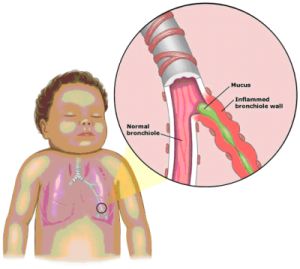
Bronchiolitis is inflammation of the bronchioles, the smallest airways of the lungs (usually less than 2 mm in diameter). The swelling and excess mucus production accompanying this infection obstructs the small airways, resulting in an audible wheeze, trapping of air in the lungs and difficulty in breathing. In severe cases this may lead to low levels of oxygen in the blood. In children under the age of 2 years this is a common respiratory infection caused by viruses. It is one of the leading causes of hospitalisation in infants and young children. In children older than two years, or adults, it usually only causes common cold-like symptoms or mild wheezing. In adults, inflammation of the bronchioles may occur in response to the inhalation of a number of dusts and gases (e.g. cigarette smoke, welding fumes, grain, silica, ammonia) or as a rare side effect of some drugs (e.g. Sulphasalazine, Penicillamine). This article will be confined to childhood viral bronchiolitis.
Magnified bronchioles (small airways) and alveoli (air spaces) of normal lungs
Causes
Bronchiolitis is caused by several viruses, the commonest by far being respiratory syncytial virus (RSV). Other viruses known to cause it - though less often - are:
Influenza
- Parainfluenza
- Adenovirus
- Coronavirus
- Rhinovirus
- Measles
Human Metapneumovirus
Small airways inflamed by RSV
RSV is transmitted through virus-containing droplets that are scattered into the air by breathing, coughing or sneezing. These droplets can also be carried on the hands for several hours, and spread infection by touching a child's eye, nose, or mouth. In South Africa RSV epidemics last 3 - 4 months and the time of year varies in different centres: Gauteng from late February to August, KZN in February and March and Cape Town usually in autumn and winter, from May to September. Infections can occur more than once, even in the same year, but repeat infections are usually milder. Nearly all children have been infected by the age of 2 years.
Risk factors
Known risk factors are:
- preterm (less than 36 weeks) babies
- infants less than 6 months old
- infants in day care
- exposure to passive smoking & pollution (solid fuels)
- overcrowding
- HIV and other immunodeficiencies
- infants and children with underlying lung or heart disease
- lack of breastfeeding
- adults who are elderly or are immunocompromised patients (leukaemia or transplant).
Symptoms and signs
There is a short incubation period of 2 - 8 days after infection. The common early symptoms are similar to the common cold:
- fever
- nasal congestion and discharge
- cough (may last for 14 or more days)
- decreased appetite
Infection of the small bronchioles is established within a day or two leading to:
- wheeze or whistling sound on breathing out (usually lasts about 7 days)
- difficulty breathing
- difficulties with feeding (because of nasal blockage and rapid breathing).
The common signs are:
- fever higher than 38ºC
- rapid breathing (60 - 80 times per minute)
- wheezing.
Signs of severe bronchiolitis include:
- nasal flaring (nostrils enlarge during breathing)
- breathing rapidly with severe difficulty
- retractions (sucking in of the skin around the ribs and the base of the throat)
- grunting
- apnoea (a pause in breathing for more than 15 or 20 seconds), which occurs more commonly in premature infants and those younger than 2 months
- blueish-tinged skin (called cyanosis) due to low oxygen levels, which is best noticed on the finger and toenails, ear lobes, tip of the nose, lips and tongue
- problems with drinking, which can lead to dehydration.
- Severe pneumonia can follow, even leading to respiratory failure. The effort required to breathe faster and harder is tiring and the child may not be able to continue to breathe on his/her own.
- Ear infections (otitis) and sinusitis may also occur.
Diagnosis
The diagnosis is clinical, based on the above symptoms and signs, and blood tests and chest X-rays are not usually necessary. The presence of the virus may be confirmed by testing airway secretions (for instance, a nasal swab). If complications or other diseases (such as added bacterial infection) are suspected, blood tests or X-rays may be done.
Treatment
In normal infants and children, RSV bronchiolitis is usually a self-limiting disease. Symptomatic and supportive treatment is provided:
- fever control with paracetamol syrup if the temperature is higher than 38ºC (Aspirin should never be given to any child <18 years)
- saline nose drops or spray followed by bulb suction in infants, or blowing in older children, to help the blocked and runny nose
- Encourage adequate fluid intake.
- monitoring the child regularly for signs or symptoms of worsening (increased rate of breathing, apnoea, worsening chest retractions, nasal flaring, cyanosis, or a inability to feed)
- Smoking around the child should be avoided because it can worsen a child's cough.
- precautions to prevent spreading the virus to other children and susceptible adults (see Prevention below).
Antibiotics are not effective in treating bronchiolitis because it is usually caused by a virus and bacterial co-infection is rare. Cough medicines and decongestants have not been proven to be helpful and are not recommended. Sedatives should not be used as they can suppress breathing efforts and lower blood oxygen.
A child who appears to be tiring, stops breathing, grunts, has cyanosis or has difficulty drinking needs urgent medical attention and hospital admission. Hospitalisation is also necessary if the child has underlying medical problems (e.g. HIV, malnutrition, heart or lung disease) or the social circumstances prevent adequate care of a sick child.
Hospital treatment for more severe infections is needed in about 3% of cases and includes:
- supplemental humidified oxygen (usually given by placing a nasal cannula or tube under a child's nose, a face mask over the nose and mouth or by placing clear plastic box over the head)
- A breathing tube (endotracheal tube) may need to be inserted into the mouth and throat and connected to a breathing machine (ventilator). This is usually only for a short time, unless complications occur.
- fluids (intravenously if the child is unable to drink)
- Nebulised hypertonic (3%) saline may be tried.
- Physiotherapy is usually unhelpful but may sometimes be used to clear secretions.
- Nebulised bronchodilators(to open the airways) are usually not effective, though may be tried as a small percentage of patient do show a limited response.
- Antivirals such as Ribavarin are only considered in immunocompromised children (e.g. after transplantation).
- Antibiotics are only used for uncommon co-existing infections such as pneumonia, otitis, urinary tract infection.
- Anti-inflammatory drugs such as inhaled or oral corticosteroids (prednisone) and Montelukast are not effective.
Outcome
Most children with bronchiolitis who are otherwise healthy begin to improve within two to five days. In some, especially younger infants, and those with underlying medical problems (e.g. asthma or another lung disease) wheezing persists for a week or more and it may take as long as four weeks for the child to return to "normal". The mortality rate for children sick enough to need hospitalisation is less than 2 percent, with more males dying than females. Hospitalised children are usually well enough to return home within three to four days.
In about 40% there is increased risk of recurrent wheezing episodes related to viral infections, but these usually end at about 3 years of age. Some studies have noted an increased risk of asthma following an episode of bronchiolitis, although it is unclear if this is due to the bronchiolitis, other risk factors (e.g. cigarette smoke) or whether bronchiolitis is just more common in those with a genetic predisposition to asthma. Viruses frequently trigger asthma attacks in children with asthma. Asthma is more likely in those with recurrent wheezing episodes, a family history of asthma or allergy, or a past history of hay fever or eczema.
Prevention
A child with bronchiolitis should be kept away from other children and susceptible adults (e.g. those with chronic heart or lung diseases or with a weakened immune system) until the wheezing and fever are gone. Use standard hygiene measures, such as hand washing and drying or alcohol-based hand rubs before and after leaving the room. Environmental decontamination may be helpful and children should not be exposed to passive smoking. Yearly influenza vaccination is recommended for all children older than 6 months, as well as their carers and contacts. Palivizumab (specific RSV monoclonal antibody) by monthly intramuscular injection may be used in premature infants (less than 36 weeks) or those under 2 years with underlying medical conditions (e.g. heart or lung disease, immunodeficiency).
Dr A.G. Hall
Reviewed by Prof Gillian Ainslie, UCT Lung Institute, September 2010




 Publications
Publications
 Partners
Partners