The management of diabetes has been consistently improved over the last half century, but now the development of insulin implants could change the face of diabetes care completely.
From the time it was discovered, diabetes has been a notoriously difficult condition to manage. The prognosis for diabetics used to be very poor with many living drastically shorter lives than the average person. Health24's Dr. Owen Wiese explains why:
"Diabetes, being a systemic disease, affects every system in the body. Uncontrolled blood sugars may make you feel sick immediately, but it is the long-term effect that uncontrolled sugars have on your eyes, heart, kidneys and other organs that can dramatically reduce your quality and length of life."
It is because of these complications that researchers are continuously developing enhanced ways to improve insulin delivery and ultimately better manage blood glucose levels. Technology is beginning to move beyond insulin injections and insulin pumps that rely on human decision-making to artificial pancreases that can act on their own, much like a human pancreas normally would.
There are a number of different companies and research labs working towards developing artificial pancreases. In fact, earlier this year the first external artificial pancreas was fitted on a 5-year-old Australian boy with type 1 diabetes. While an artificial pancreas can exist externally, researchers are now working towards devices that can be implanted into the body, giving the patient as close to normal a life as possible.
InSmart artificial pancreas

Image courtesy of Renfrew Group International
One form of implantable device was developed by Professor Joan Taylor through De Montfort University in Leicester, United Kingdom. This little device is approximately the size of a wristwatch and is implanted into the abdomen of the patient. It contains a gel barrier that reacts in response to increasing blood glucose levels in the blood, and releases insulin accordingly.
Unfortunately the gel reservoir only lasts two weeks before it needs to be filled again. This has to be done via an external port on the outside of the body. Insulin injected into the port fills the reservoir again.
This product is due to be tested in human trials during 2016. Should the trials prove successful, it is expected that the product will become available within the next decade. Read more about that here.
While this product is certainly a dramatic breakthrough and will undoubtedly significantly improve diabetes management, it still requires a port on the outside of the body for the insulin reserve to be topped up.
Another device could eliminate this entirely...
VC-01 combination product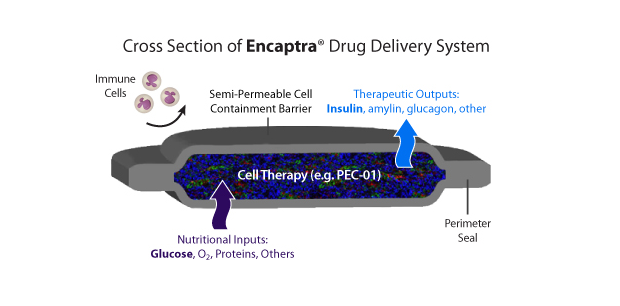
Image courtesy of ViaCyte
Another exciting product that is currently being developed is the VC-01 by Viacyte. This ingenious little device contains stem cells capable of producing insulin.
ViaCyte is not the only group to achieve this. Towards the end of 2014, Health24 reported that Professor Doug Melton and his team from Harvard University had succeeded in creating insulin-producing stem cells. Unfortunately, placing these cells into the body as they are will only temporarily solve the problem.
The biggest challenge in implanting these cells is the body's own immune system. With type 1 diabetes, the body attacks the insulin-producing beta cells. Simply replacing the destroyed beta cells with new stem cells will only work temporarily until the body manages to destroy those too.
What ViaCyte has managed to do is protect the stem cells from the immune system by placing them in a capsule, known as the Encaptra drug delivery system. The entire capsule is then implanted into the patient and, in theory, functions in a very similar way to a human pancreas. The stem cells are capable of differentiating and producing more cells, the ViaCyte website explains. The VC-01 falls into a category of bioartificial pancreases.
Clinical trials are currently under way and, to date, the device has been implanted in four humans and will be implanted into a further 36 people by the end of 2016. ViaCyte CEO, Paul Laikind indicates that if all goes according to plan, they will be moving towards getting the VC-01 device on the market in five years' time, according to an interview with Knoepfler Lab.
Read: Technology lightens the burden of diabetes
Treatment vs. cure
While these products will eventually be able to regulate the administration of insulin and blood glucose monitoring without much human intervention, they will not cure diabetes. There is a difference between managing and curing a condition. These devices merely aim to improve upon the management of the condition by improving blood glucose control.
Until the time that scientists discover how to "switch off" the immune response that attacks the pancreatic cells, type 1 diabetes will carry on existing.
Read more:
Why isn't there any cheap, generic insulin?
Islet transplant for diabetics
Cost of diabetes skyrockets in the U.S
Image: Stem cell research in the PCR strip from Shutterstock




 Publications
Publications
 Partners
Partners










