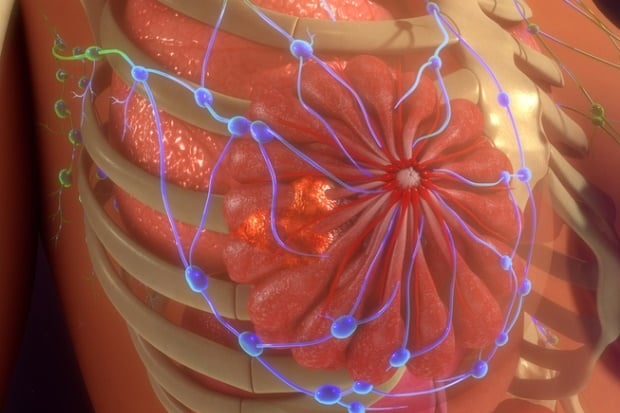
Breast cancer is the most common invasive cancer in women and makes up 16% of all female cancers worldwide.
A drug called Xeloda can extend the lives of some women whose breast cancer is not wiped out by standard treatment, a new clinical trial finds.
Oncologists said the results are "practice-changing".
The results were published in the New England Journal of Medicine.
"This drug is already approved, and we've been using it for a long time in cancer treatment," said Dr Stephen Malamud, an oncologist at Mount Sinai in New York City.
Approved for advanced breast cancer
Xeloda (capecitabine) is a pill, so it's easy to take and is "much less toxic" than standard chemotherapy, noted Malamud, who was not involved in the new research.
"Most importantly," he said, "it extended overall survival in this study."
In 1998, Xeloda was approved in the United States for advanced breast cancer that had spread to distant sites in the body. The new trial, done in Japan and South Korea, tested the drug for a different group of patients.
It focused on 910 women whose breast tumours were not completely eliminated by standard chemotherapy and surgery. In addition, they all had cancer that lacked a protein called HER2 – which meant they could not benefit from breast cancer drugs that target HER2, such as Herceptin.
iStock
Those women have a fairly high risk of seeing their cancer progress, according to the researchers on the trial, led by Dr Masakazu Toi, of Kyoto University in Japan.
Not a panacea
In the study, Xeloda improved those odds. It cut patients' risk of relapse or death by 30% over five years.
At that point, 74% were still alive and recurrence-free, versus just under 68% of women who'd received placebo pills in addition to standard treatment.
"It's not a panacea, by any means," Malamud said. "But it's a nice 'back door' treatment to improve women's outcomes."
Dr Elizabeth Comen is a medical oncologist at Memorial Sloan Kettering Cancer Center in New York City. She said doctors have already begun using Xeloda for women like those in the trial, based on preliminary reports. (The trial was actually stopped early, in 2015, when it became clear that Xeloda had benefits.)
"This is a landmark trial," Comen said. "It really is, in my opinion, practice-changing."
Mammogram every year
The women in the study all had breast tumours that had not yet spread to distant sites in the body. But many had cancer in nearby lymph nodes.
They'd all received standard chemotherapy before surgery, but still had "residual" cancer left behind.
CANSA (the Cancer Association of South Africa) advocates a mammogram every year for all women from age 40 for purposes of non-symptomatic breast screening.
CANSA further advocates that:
- Women who are at risk and those that have had breast health problems in the past should consult their respective health professional to determine a schedule applicable to them.
- Women aged 40 to 54 should have an annual mammogram.
- Women 55 years and older should change to having a mammogram every two years – or have the choice to continue with an annual mammogram.
- Screening should continue as long as a woman is in good health and is expected to live 10 years or longer.
- Every woman should be informed of the known benefits, limitations, and potential harms linked to breast cancer screening by means of a mammogram.
Side effects
Toi's team randomly assigned the patients to one of two groups. Most women in both groups received radiation, and those with hormone-sensitive breast cancer started on hormonal medications.
Only one group received Xeloda, while women in the other group were given placebo pills. The treatment was given in six or eight three-week "cycles," with two weeks on the drug, one week off.
Five years later, 89% of Xeloda patients were still alive, compared with just under 84% of placebo patients.
The main side effect – affecting almost three-quarters of patients – was hand-foot syndrome. That's a reddening and swelling of the palms and soles of the feet. It's similar, Malamud said, to a "bad sunburn", and it goes away once the drug is stopped.
The trial was funded by the Advanced Clinical Research Organization and Japan Breast Cancer Research Group.
Read more:




 Publications
Publications
 Partners
Partners